Abstract
The results of the PRIMA trial published a decade ago, substantiated the benefit of maintenance therapy with anti-CD20 monoclonal antibodies (MoAb), following chemo-immunotherapeutic induction, for prolongation of the progression-free survival (PFS) of patients with high-tumor- burden follicular lymphoma (FL). Rituximab-associated delayed neutropenia, defined as an event occurring after recovery of cytopenias related to the chemotherapy backbone, has been reported in lymphoma patients, with the prevalence varying between 8-27%. Several mechanisms have been implicated in its pathogenesis, mainly related to B-cell recovery, such as a disrupted stromal-derived factor-1 gradient and the generation of anti-neutrophil antibodies. The available data associated with anti-CD20 MoAb-mediated delayed neutropenia during the prolonged (2-year) maintenance treatment in FL are limited, and the consequences of its occurrence remain unclear. The aims of this study were to assess the prevalence of neutropenia and risk factors for its development in FL patients during maintenance therapy as well as to evaluate its severity and impact on decisions regarding modification of the original treatment protocol.
In this retrospective study, clinical data were retrieved from electronic medical records of FL patients treated at the Rambam Health Care Campus between 2006 (when maintenance therapy was first applied) and 2021.
Continuous variables were statistically processed using the Mann Whitney U test and categorical variables - using Fisher exact tests. Statistical significance was defined as p <0.05.
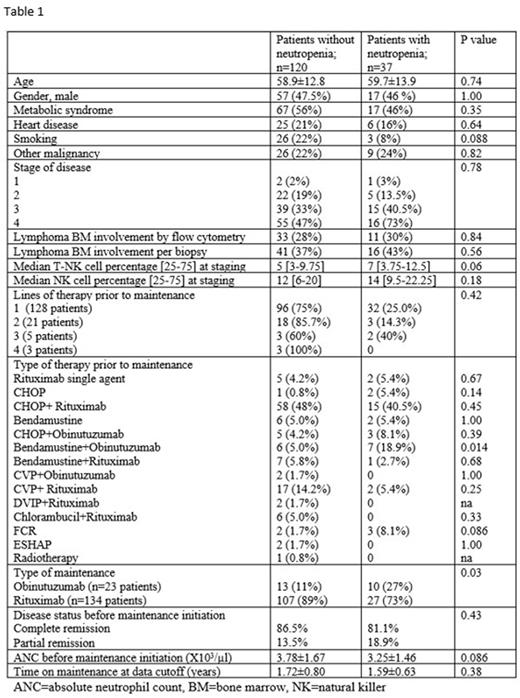
During the study period, a total of 305 patients treated for high-tumor-burden FL were identified in the institutional database; 164 of these patients (53.8%) also received maintenance therapy with anti-CD20 MoAb (rituximab or obinutuzumab). Data on 157/164 patients were included in the final analysis after the exclusion of 7 patients due to their concomitant autoimmune disease. During maintenance therapy, 37/157 (23.6%) patients developed delayed neutropenia, with 4/37 (11%) of them experiencing at least one recurrent event. This relatively high percentage of delayed events is comparable only to that observed in a study which evaluated heavily pretreated lymphoma patients (Cattaneo C et al. Leuk Lymphoma, 2006), exposed to highly myelotoxic regimens or fludarabine and did not include a maintenance phase. Median time from the start of maintenance to the first neutropenic episode in the current study was 5 (range 1.5-12) months and the majority of these events were of high grade (III and IV in 24% and 38% of patients, respectively). Despite the fact that 15/37 (40%) patients who developed this complication were hospitalized with neutropenic fever, the occurrence of neutropenia led to early discontinuation of maintenance treatment solely in 14% of the cohort and had no effect on PFS, measured at a median follow-up of 91.5 months. Univariate and multivariate analyses identified the use of the obinutuzumab/bendamustine (O/B) combination for induction therapy, or maintenance with obinutuzumab (O) as the only risk factors of delayed neutropenia development in patients on maintenance therapy (odds ratios in case of O/B induction followed by O maintenance: 4.433 [95%CI=1.387-14.17, p=0.012]; in case of O maintenance: 3.048 [95%CI=1.207-7.697, p=0.018]). All other laboratory and clinical factors examined did not impact late neutropenia occurrence (Table 1).
The current study demonstrates that the administration of obinutuzumab both as part of induction with bendamustine and as maintenance therapy increases the likelihood of developing anti-CD20 MoAb-induced delayed neutropenia, suggesting that pharmacokinetic differences between type I and type II MoAb are partly responsible for this effect. Moreover, the findings regarding the prevalence of neutropenia and time to its first episode in this study cohort do not support the involvement of processes related to B-cell recovery in the pathogenesis of this complication during maintenance treatment, and warrant investigation of alternative mechanisms. The risk factors for delayed neutropenia in FL patients on maintenance therapy, identified in this study, should be considered in the treatment paradigm for older frail patients who are more prone to complications of neutropenic fever.
Disclosures
Zuckerman:Orgenesis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BioSight Ltd: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Cellect Biotechnology: Honoraria, Speakers Bureau; Janssen: Honoraria, Speakers Bureau; Novartis: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal